The Sacroiliac joint (commonly referred to as SIJ) lies next to the spine and connects the sacrum with the pelvis (iliac crest). It is a strong, weight bearing joint that acts as a shock-absorbing structure for all the forces of the upper body.
‘Sacroiliac Joint Dysfunction’, is a problem that we treat and rehbailitate Using physiotherapy. This is a broad term that refers to the abnormal biomechanical function of the Sacroiliac joint.
The role of physiotherapy and the assesment of the SIJ in a physiotherapy setting
Physiotherapy interventions are effective in reducing pain, disability and restoring pelvic position in Sacroiliac dysfunction ( Al-subahi et al. 2017).
most commonly we find a history of;
- trauma (trip, fall or impact)
- pregnancy (hormonal changes lead to changes in posture and ligament stability),
- lumbar pathology (lower back pain, can causes changes in posture or movement control) ,
- or lumbar fusion surgery (changes in posture and biomechanics in the lower back).
The incidence of lower back pain originating from the sacroiliac joint may be as high as 27% in the general population and can often be mis diagnosed without an indepth assesment.
Our goals are
- Return the SI joint to its normal position and maintain this position.
- Optimal SI joint function occurs with the SI Joint in neutral (mid-range) position therefore we strive to achieve this through treatment and exercise/postural re education.
- Restore optimal alignment of the lumbar spine, sacroiliac joint and hip joint
- Optimise functional stability of the lumbopelvic region by restoring normal function of the supporting muscles such as the hip stabilisers and deep core muscles
Key answers that our assessment will find:
OUr main goal is to Isolate the SIJ as the driver of pain through our history taking and special tests, eliminating other joints such as;
-
-
- Lower back
- Hip
-
We will also assess factors contributing to the sacro-iliac pain/dysfunction, issues such as;
-
-
- General Deconditioning
- Weakness of stabilising (Core) Musculature
- Imbalance of muscle length or strength on the muscles that attach to the legs or cross the trunk and pelvis ( remember there are 35 that attach onto that pelvic structure!)
- Problems with function, position or motion in the joints above and below the SI joint including the hips and spine directly above and below but also including joints at a distance like the ankle.
- Restriction or scarring in the muscles or tissues that overlay or attach to the SI joint
- Poor postural patterns and asymmetrical movement patterns with daily activities
- Abnormal or asymmetric gait
- Lack of control of the muscles that coordinate to stabilise the lower back and pelvic region (often called motor control)
- Pain in soft tissues and joints other than and including the SI joint.
-
Your assessment of the SIJ at Movement Perfected will include to following tests – here’s how and why we do these tests
The Stork Test
The stork test is a motion-control test where both form and force closure mechanisms are assessed by observing how load is managed through the pelvis in standing.
The ability to maintain a stable alignment of the ilium relative to the sacrum when testing the weight-bearing side (self-braced alignment of the pelvic bones) is what is expected. There should be no relative movement occurring in the pelvis during this load-transfer test.
Active Straight leg raise ( ASLR)
This test assesses load through the pelvis in a supine position.
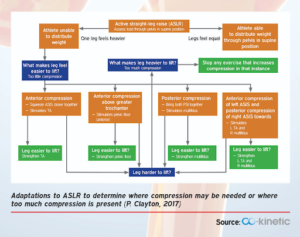
- Anterior compression – squeezing the ASIS closer together (simulates transversus abdominis (TA). If the leg is easier to lift as a result it would mean we would ensure specific TA activation is incorporated into rehabilitation.
- Anterior compression above the greater trochanter of the hips (simulates anterior pelvic floor) If the leg is easier to lift as a result it would mean we would ensure specific pelvic floor activation is incorporated into rehabilitation.
- Posterior compression – bringing both PSIS together (simulates multifidus).) If the leg is easier to lift as a result it would mean we would ensure specific multifidus strengthening is incorporated into rehabilitation
- Anterior compression of left ASIS and posterior compression of right PSIS toward each other (simulates left TA and right multifidus). If the leg is easier to lift as a result it would mean we would ensure specific left TA and right multifidus Strengthening is incorporated into rehabilitation
Standing Flexion Test
During the standing flexion test, the physiotherapist will notice any reduced mobility in the affected joint, which will be noticeable when performing the standing flexion test. It is important to note that the standing flexion test alone is not enough to diagnose SIJD as it is less sensitive.
Technique:
- The patient stands erect, with his feet at shoulder width.
- The therapist stands or squats behind the patient and places his thumbs directly under each posterior superior iliac spine (PSIS).
- The patient bends forward, starting with flexing the neck, then the upper thoracic spine to the lumbar spine, and as far as possible while keeping the knees extended. The therapist will observe each PSIS and their movement. Each PSIS should move an equal amount in a superior direction. If one PSIS moves further cranial than the other, the test is positive.
- The side with the greater movement is the affected side, because an articular restriction between the ilium and sacrum occurs. The sacrum will bend forward along with the lumbar spine, and if there is an articular restriction in the SIJ, nutation will occur less in that joint than on the other side.
Because similar findings may occur in case of contralateral hamstring tightness, this condition should be examined too to rule out any effect of tightness
Seated flexion test
The seated flexion test is used to detect sacroiliac joint (SIJ) dysfunction. The patient is seated with the therapist positioned behind the patient.
Technique:
- The therapist places his thumbs on each posterior superior iliac spine (PSIS) and the patient is asked to flex the trunk as far as possible.
- The test is negative if the movement of the PSISs was symmetrical or positive if one side moved more than the other in the cephalic and/or ventral directions.
- A positive result indicates limited movement of the sacrum on the ilium, and therefore limited SIJ motion on the side of the superior PSIS.
Assessment of the psoas on the Sacro iliac joint
Hu et al. (2011) investigated the role of the psoas in hip flexion using the Active Straight Leg Raise ( ASLR) test which we use in clinic along with compression forces applied manually to further differentiate where the issues lies within the SIJ and where we need to be specific with our rehabilitation programme. The psoas is noted to be active bilaterally in the ASLR test- reflecting its’ stabilising effect of the lumbar spine).
The addition of compression to the pelvis as mentioned as part of the assessment (squeezing of the anterior portion of the innominates, or bringing the ASIS closer together) during the ALSR can enable the leg to be lifted with ease (unless there is already too much compression, in which case this movement may be made even more difficult.
The diagram below explains how through a thorough examination of the SIJ and applying pressures in certain areas around the SIJ enables us at Movement Perfected to individualise the rehabilitation programme based on the results of these compressions during the ASLR test. The compression that is noted to be most helpful for the patient during the ASLR test should be noted and kept in mind when planning the treatment plan.
IN SUMMARY
Adaptations as the result of injury in the sacroiliac joint, often result in muscle imbalances, the identification of which is necessary for appropriate treatment. We at Movement Perfected pride ourselves on trying to be as specific as we can in our assessment to ensure the best treatment plan for each individual is created and implemented. There are two key points to consider when assessing the SIJ 1) the SIJ as a load-transferring mechanical junction between the pelvis and the spine that may cause either the SIJ or the associated structures to produce pain (SIJ dysfunction), and the SIJ joint structures as a source of pain (SIJ pain). Movement dysfunction of the lumbar spine, hip and pelvis along with neurodynamics are key to being assessed properly for fast and effective rehabilitation. That is what we will assess fully at Movement Perefcted- to not only resolve the pain and dysfunction but also to prevent reoccurance.
